Pregnancy is often described as a miraculous journey filled with hope and joy. However, for many women, it can also be a time of great anxiety, especially regarding the possibility of miscarriage. Early pregnancy loss, while difficult to talk about, is a reality that many women face. In this blog, we aim to provide support and information to those navigating this challenging experience.
What is a Miscarriage?
A miscarriage, also known as spontaneous abortion, is the loss of a pregnancy before the 20th week. It can occur for various reasons, many of which are beyond anyone’s control. While it’s a common occurrence, affecting approximately 10-20% of known pregnancies, it can leave significant emotional and physical impacts on those involved.
Why Do Miscarriages Happen?
Understanding the reasons behind a miscarriage can be complex. Potential causes include:
Chromosomal Abnormalities:
The most common reason for early pregnancy loss is chromosomal abnormalities in the developing embryo. These issues often occur by chance and are not usually indicative of a larger problem.
Hormonal Imbalances:
Hormonal imbalances can have a significant impact on embryonic development and overall reproductive health. Low progesterone levels, in particular, are critical to maintaining a healthy pregnancy. Here’s a deeper look into how hormonal imbalances, specifically low progesterone, can affect embryo development:
Importance of Progesterone:
Hormonal imbalances can have a significant impact on embryonic development and overall reproductive health. Low progesterone levels, in particular, are critical to maintaining a healthy pregnancy. Here’s a deeper look into how hormonal imbalances, specifically low progesterone, can affect embryo development:
Importance of Progesterone:
- Support of Luteal Phase: Progesterone is produced after ovulation by the corpus luteum and is essential for preparing the uterine lining (endometrium) for implantation of the embryo.
- Embryo Development: Progesterone helps maintain the uterine lining and prevents its breakdown, which is crucial for the fertilized egg to implant and grow.
- Immune Modulation: Progesterone also plays a role in modulating the immune response, allowing the body to tolerate the embryo, which is genetically distinct from the mother.
Effects of Low Progesterone:
- Inadequate Uterine Lining: Low levels of progesterone can result in a poorly developed endometrium, which may not be able to support and nourish the implanting embryo.
- Increased Risk of Miscarriage: Insufficient progesterone can lead to an increased risk of miscarriage, particularly in the early stages of pregnancy.
- Hormonal Disruption: Low progesterone may indicate underlying hormonal imbalances, such as issues with the hypothalamus, pituitary gland, or ovarian function. These imbalances can affect overall fertility and reproductive health.
Uterine Abnormalities:
Uterine abnormalities can significantly impact reproductive health and contribute to miscarriage. Here’s a closer look at how structural issues in the uterus can affect pregnancy outcomes:
Types of Uterine Abnormalities
Fibroids:
- Definition: These are non-cancerous growths (leiomyomas) of the uterine muscle tissue.
- Impact on Pregnancy: Depending on their size and location, fibroids can distort the uterine cavity, interfere with implantation, and restrict fetal growth. Submucosal fibroids (those that grow into the uterine cavity) are often of particular concern as they can impede embryo implantation and lead to miscarriage.
Uterine Septum:
- Definition: This is a congenital anomaly where a fibrous or muscular tissue septum divides the uterine cavity.
- Impact on Pregnancy: A septate uterus can lead to recurrent miscarriages due to inadequate space for the developing embryo and increased risk of placental complications.
Bicornuate Uterus
- Definition: This is a heart-shaped uterus caused by incomplete fusion of the Müllerian ducts during fetal development.
- Impact on Pregnancy: A bicornuate uterus can lead to complications such as preterm labor, malpresentation of the fetus, and miscarriage, especially if the pregnancy occurs in one of the horns.
Unicornuate Uterus:
- Definition: This is a congenital condition where only one side of the uterus develops properly.
- Impact on Pregnancy: It can result in an increased risk of miscarriage, as well as complications like ectopic pregnancy or preterm labor.
Asherman’s Syndrome
- Definition: This condition involves the formation of scar tissue (adhesions) in the uterine cavity, often as a result of previous surgeries like dilation and curettage (D&C).
- Impact on Pregnancy: Asherman’s Syndrome can lead to reduced uterine capacity, increasing the risk of miscarriage, abnormal placentation, and complications with future pregnancies.
Uterine abnormalities play a significant role in reproductive health and can lead to miscarriage through various mechanisms. It is essential for individuals experiencing recurrent pregnancy loss or fertility issues to consult with a healthcare provider for thorough evaluation and tailored treatment options. Early intervention and management can enhance the chances of a successful pregnancy.
Health Conditions
Chronic health conditions can significantly impact fertility, pregnancy outcomes, and the likelihood of a successful pregnancy.Here’s an overview of some common health issues and their effects on pregnancy:
Diabetes
Types: Both Type 1 and Type 2 diabetes can affect pregnancy.
Impact on Pregnancy: Poorly controlled diabetes increases the risk of miscarriage, congenital anomalies, preterm labor, and complications like gestational hypertension. High blood sugar levels can affect fetal growth and development, leading to conditions such as macrosomia (large baby) and increased risk of perinatal mortality.
Management: It is crucial for individuals with diabetes to maintain good blood sugar control before and during pregnancy. This may involve regular monitoring of blood glucose levels, adjustments in medication, diet, and exercise, and close collaboration with healthcare providers.
Autoimmune Disorders
Examples: Conditions such as lupus, rheumatoid arthritis, antiphospholipid syndrome, and thyroiditis fall under this category.
Impact on Pregnancy: Autoimmune disorders can lead to increased risks of miscarriage, preterm birth, and complications related to placental function. For example, antiphospholipid syndrome can cause blood clotting issues that may impede blood flow to the placenta.
Management: Women with autoimmune disorders should work closely with their healthcare team to manage symptoms and monitor pregnancy closely. Treatment may involve medications to control immune responses while ensuring safety for both the mother and fetus.
Thyroid Disorders
Types and Management:
Hypothyroidism: Requires careful monitoring of thyroid hormone levels, with potential adjustments in medication during pregnancy to maintain proper levels and support fetal development.
Hyperthyroidism: Management with antithyroid medications and monitoring is crucial to prevent complications for both mother and baby.
Obesity
Impact and Management:
Addressing obesity through lifestyle changes, including a balanced diet and exercise, can greatly reduce risks associated with either infertility or complications during pregnancy. A multi-disciplinary approach—working with physicians, dietitians, and exercise specialists—often yields the best results.
Chronic Hypertension
Impact and Management:
Regular monitoring and control of blood pressure are essential prior to and throughout pregnancy. Safe medications may be prescribed to manage hypertension effectively and minimize complications.
Mental Health Conditions
Impact and Management:
Acknowledging and addressing mental health concerns is essential. Having access to therapy, counseling, and support networks can greatly enhance the emotional well-being of individuals during pregnancy.
Lifestyle Factors
Smoking, Alcohol, and Drugs: Education on the risks associated with these behaviors is vital. Programs and support to help individuals quit or reduce use can significantly improve pregnancy outcomes.
Age
Maternal Age and Miscarriage Risks: Understanding that women over 35 may face increased risks due to declining egg quality can guide planning and discussions with healthcare providers about options for conception.
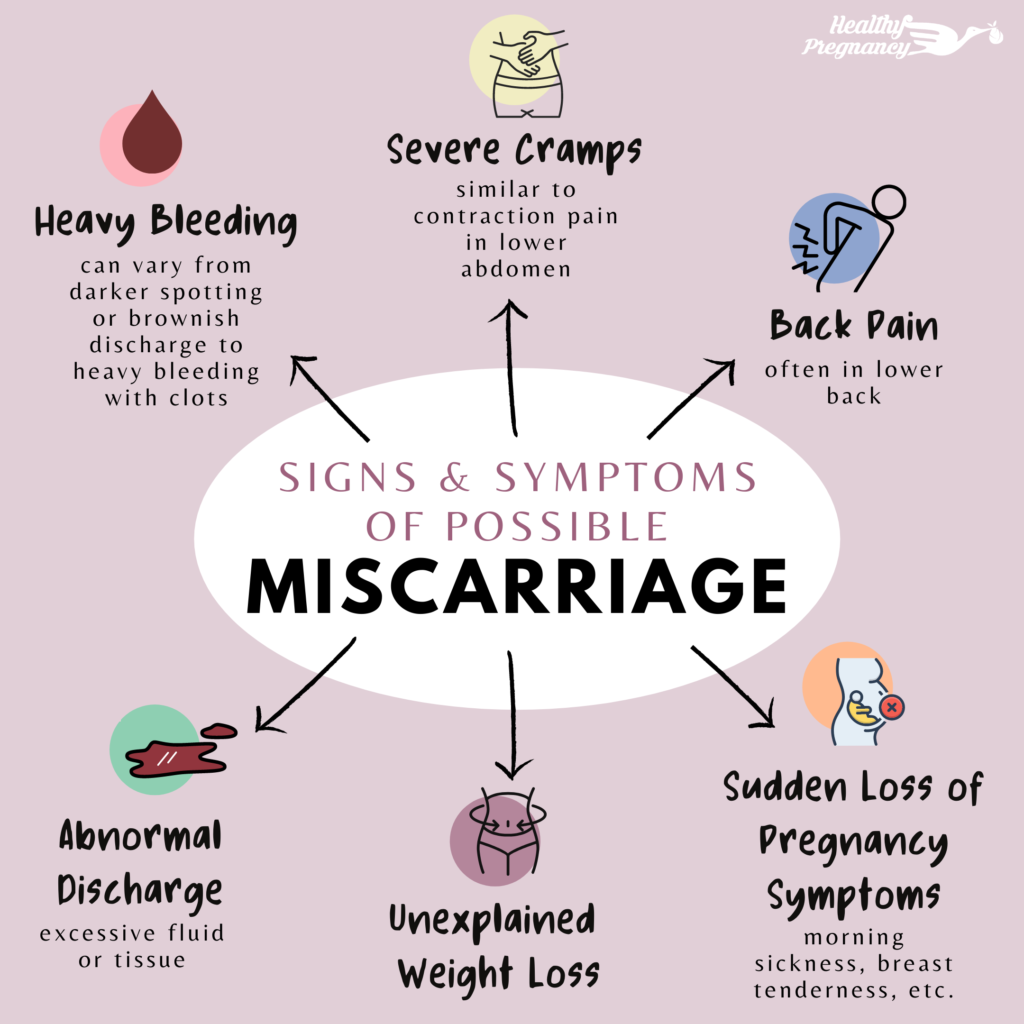
Recognizing Signs of Miscarriage
Early awareness of symptoms (such as vaginal bleeding, cramping, and the passage of tissue) can facilitate prompt medical attention, which may be critical in some cases.
Coping with Emotional Aftermath
Acknowledgment and Support: Validating feelings of grief is essential, and connecting with others who have experienced similar losses can foster healing. Creating memorials is a thoughtful way some find peace and recognition of their loss.
Moving Forward
It’s important for individuals who have experienced a miscarriage to talk with their healthcare providers about future pregnancy plans, as many are able to conceive and carry to term successfully after such losses.

Closing Thoughts
Miscarriage remains a difficult and often stigmatized topic. By fostering open dialogue and support networks, society can provide compassion and healing for those who are affected. Encouraging conversations around miscarriage and pregnancy loss helps normalize the experience and offers validation for those grieving, reminding them that they are not alone.
Support Resources
If you or anyone you know is navigating these issues, consider reaching out to support groups, mental health professionals, or fertility specialists to obtain tailored assistance and care. It’s crucial to have a supportive network while coping with the various challenges and emotions that accompany pregnancy and its potential complications.
Thank you for bringing awareness to these important topics surrounding pregnancy, health conditions, and emotional well-being.
Discover more from fuel for life
Subscribe to get the latest posts sent to your email.
