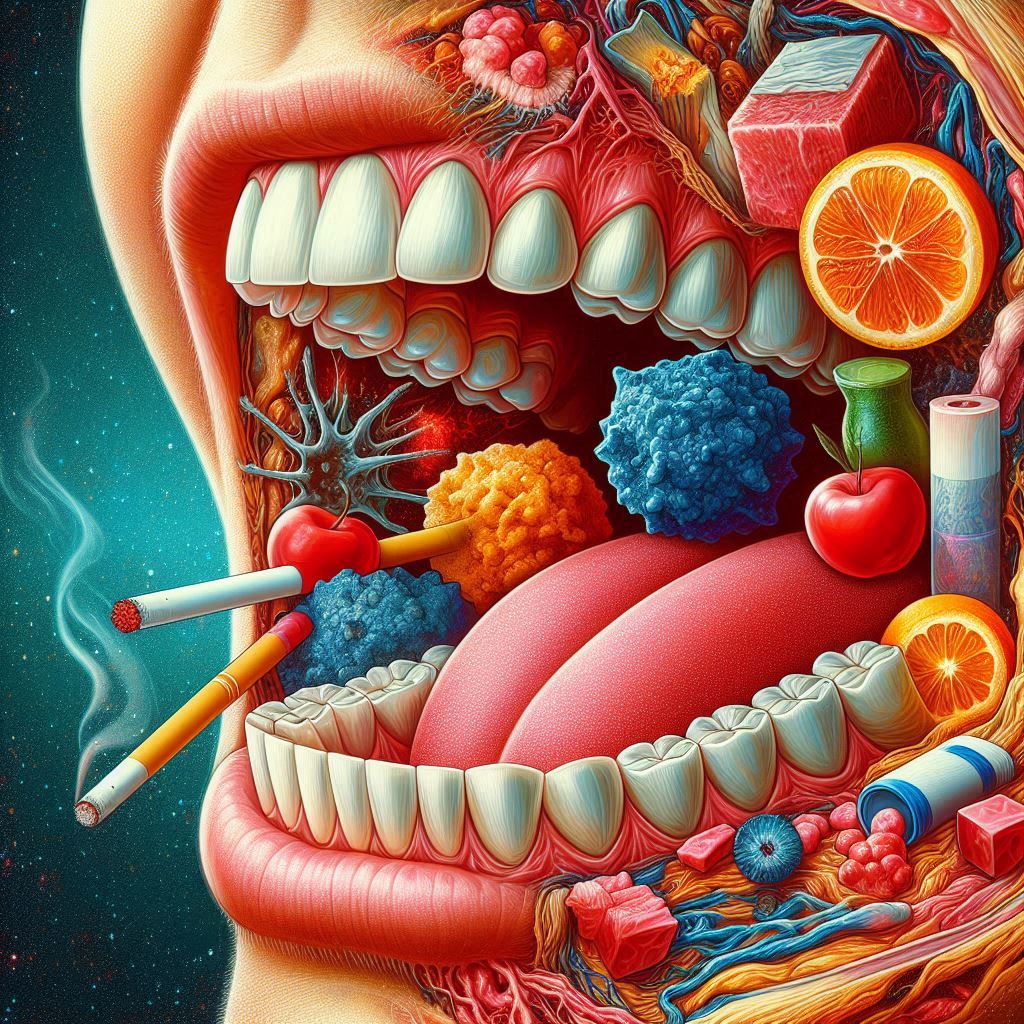
What Is Oral squamous cell carcinoma (OSCC)?
Understand the Immune Microenvironment of Oral Cavity Carcinomas Oral cavity carcinomas, especially oral squamous cell carcinoma (OSCC), are the most common head and neck cancers. These tumors are complex and involve more than just cancer cells. They contain various cellular components, including immune and stromal cells. These components are crucial for tumor progression and immune evasion. This blog will explore the immune microenvironment in oral tumors. It will also discuss innovative approaches to improve anticancer immunity. The Composition of Oral Tumors Oral tumors are not solely composed of malignant cells; they harbor diverse cellular populations that can influence the tumor’s behavior. Among these, anticancer immune cells like cytotoxic CD8(+) T lymphocytes (CTLs) and natural killer (NK) cells are essential for mounting a robust immune response against cancer cells. These immune cells infiltrate the tumor microenvironment and are pivotal in recognizing and destroying malignant cells. However, the effectiveness of these immune responses is frequently dampened by various suppressive mechanisms within the tumor microenvironment. Regulatory T cells (Tregs), macrophages, and myeloid-derived suppressor cells (MDSCs) play significant roles in immunosuppression. They contribute to an environment that favors tumor growth. This immunosuppressive milieu helps the tumor evade immune detection. Understanding the intricate dance between these diverse cell types is crucial for devising effective treatments. The Role of Immune Cell Infiltration Research has shown that the presence and activity of T and NK cells within the tumor microenvironment significantly influence the outcomes of immunotherapy, chemotherapy, and radiotherapy. Tumors with a higher infiltration of CD8(+) T cells generally respond better to these treatment modalities. However, the interplay between these immune cells and the tumor’s supporting cells can lead to altered therapeutic responses. On the flip side, many cancer therapies can inadvertently enhance the recruitment or activity of immunosuppressive cells, leading to a paradoxical worsening of the immune response against the tumor. Therefore, understanding the balance of cellular components in the microenvironment is vital to developing successful treatment strategies. Enhancing Anticancer Immunity One promising avenue for combating oral cancers is boosting anticancer immunity by targeting the tumor microenvironment. This dual approach includes enhancing the activity of immune cells while simultaneously inhibiting the function of immunosuppressive cells. Various strategies are being explored, such as immune checkpoint inhibitors, therapeutic vaccines, and adoptive cell transfer therapies. Furthermore, there is growing interest in the use of nanoparticles for targeted drug delivery. These nanocarriers can encapsulate therapeutic agents, including immune-modulating drugs, and facilitate their delivery directly to the tumor site. By doing so, nanoparticles can enhance the local concentration of anticancer agents while minimizing systemic side effects. You can Visit Also HERE Therapeutic Targets and Emerging Agents The emergence of innovative therapeutic targets and agents is transforming the treatment landscape for oral cancers. Nanoparticles, for instance, can be engineered to deliver not only traditional chemotherapy drugs but also biologics capable of modulating the immune response directly. Drugs that can enhance the activation of T cells or inhibit the function of Tregs and MDSCs represent exciting therapeutic candidates. Moreover, natural products with known anti-tumor properties are also garnering attention. Compounds from plants and natural sources can effectively modulate the immune response to cancer . As we learn more about the immune microenvironment, we can better utilize these natural products. Integrating them into therapeutic regimens may provide synergistic effects. Future Perspectives Looking ahead, the field of cancer therapy is poised for an exciting evolution. The development of combination therapies that include immune modulators and nanoparticles, alongside conventional treatments, shows significant promise for boosting anticancer immunity in oral tumors. These innovative approaches aim to enhance the efficacy of treatments by addressing immune suppression within the tumor microenvironment. Moreover, ongoing research into the mechanisms of immune suppression can lead to personalized treatment strategies, allowing therapies to be tailored to the specific immune landscape of each patient’s tumor. This personalized approach could improve treatment outcomes and make therapies more effective against oral cancers. In conclusion, comprehending the complex interactions within the immune microenvironment of oral cavity carcinomas is key to developing effective therapies. By harnessing the power of the immune system and targeting the factors that suppress it, we can move closer to more successful, targeted treatments for patients battling oral cancer. The future looks hopeful as researchers and clinicians continue to explore innovative strategies to enhance anticancer immunity and improve patient outcomes.