What Is the Role of CRT : LBBB and Cardiomyopathy
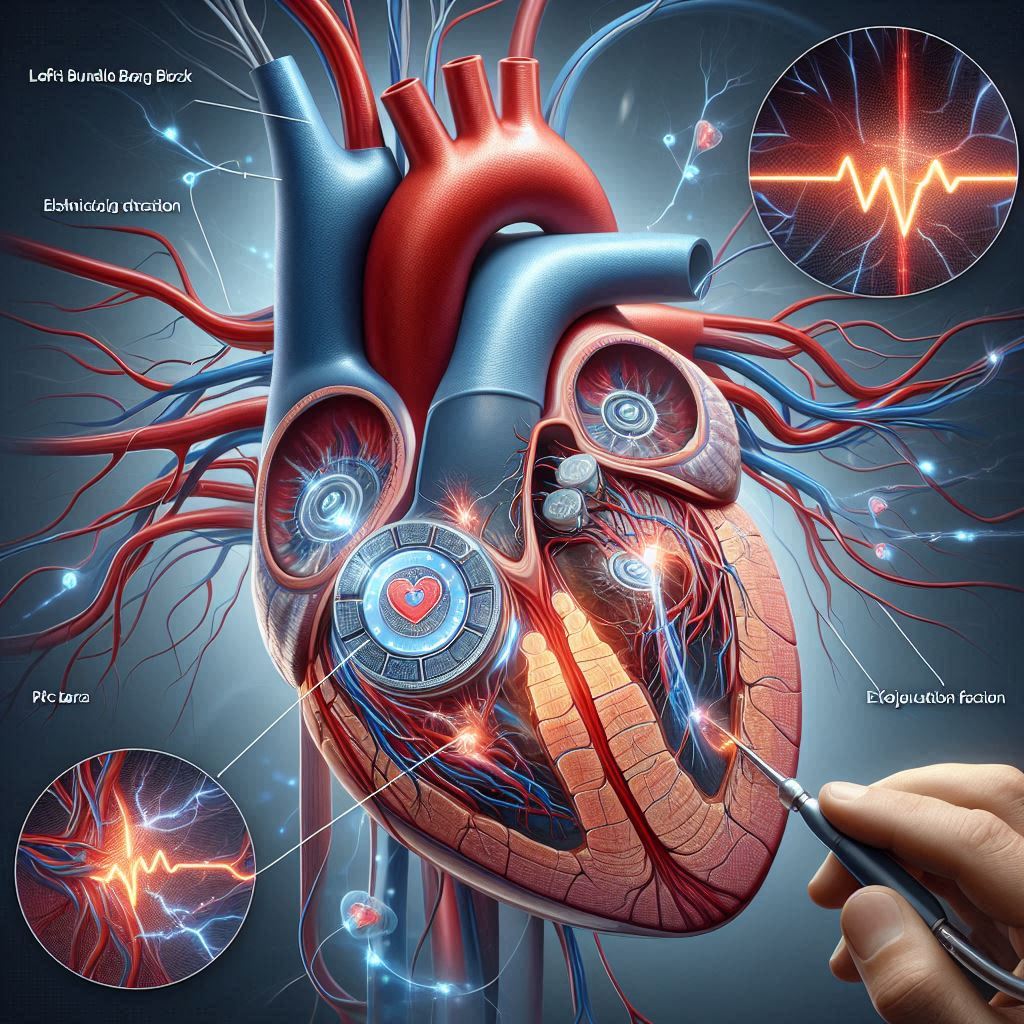
Left Bundle Branch Block (LBBB) is a condition where the electrical signals in the heart are disrupted, causing delayed or uncoordinated contraction of the left ventricle. This can lead to symptoms like fatigue, shortness of breath, and heart failure. Cardiomyopathy refers to diseases of the heart muscle that affect its size, shape, and ability to pump blood effectively. Together, LBBB and cardiomyopathy can significantly impair heart function. Cardiac Resynchronization Therapy (CRT) plays a crucial role in managing these conditions. By delivering targeted electrical impulses to both ventricles, CRT helps synchronize their contractions, improving overall heart function and alleviating heart failure symptoms. This therapy can enhance patients’ quality of life and reduce hospitalizations associated with heart failure. Understanding the Connection Between LBBB and Cardiomyopathy Left Bundle Branch Block (LBBB) is a heart condition affecting electrical conduction. It disrupts signals to the left ventricle. LBBB is often linked to structural heart disease. It is associated with increased morbidity and mortality rates. When LBBB occurs in patients with cardiomyopathy, the risks amplify. Cardiomyopathy is defined by an ejection fraction of less than 35%. This combination leads to a precarious situation for patients. Effective management of both conditions is essential for improving outcomes. Current medical guidelines recommend a standard protocol. Doctors should initiate three months of medical therapy for patients with LBBB and cardiomyopathy. After this period, they can consider cardiac resynchronization therapy (CRT). However, emerging research raises concerns. Many patients do not respond adequately to medical therapy alone. A significant percentage still require CRT even after the treatment period. This highlights the need for timely evaluation. Relying solely on medical management may delay effective treatment. Individualized assessment is essential for optimizing patient care. Certainly! Let’s dive into a more detailed explanation of Cardiac Resynchronization Therapy (CRT), especially in the context of left bundle branch block (LBBB) and its impact on cardiomyopathy. Understanding Cardiac Resynchronization Therapy (CRT) What is CRT? Cardiac Resynchronization Therapy (CRT) is a specialized treatment for heart failure patients. It is particularly effective for those with conduction system abnormalities like LBBB. CRT involves implanting a device similar to a pacemaker. This device delivers electrical impulses to both the left and right ventricles. The dual stimulation promotes synchronized contractions of the heart muscles. As a result, cardiac efficiency improves, leading to better heart function. CRT can enhance overall quality of life for patients. How Does CRT Work? In a healthy heart, the electrical signals that prompt the heart to beat travel through a well-coordinated pathway, ensuring that all chambers of the heart contract efficiently at the right times. However, in patients with LBBB, this pathway is disrupted, which leads to asynchrony; one side of the heart may contract at a different time than the other. This can result in less effective pumping action, ultimately worsening heart failure symptoms. CRT alleviates this problem by synchronizing the contractions of both ventricles. By using biventricular pacing (stimulation of both the left and right ventricles), CRT helps improve the timing of contractions—allowing for better overall blood flow and increased cardiac output. The Reversibility of LBBB-Associated Cardiomyopathy What is LBBB-Associated Cardiomyopathy? LBBB can lead to a form of heart failure known as LBBB-associated cardiomyopathy, where the pumping ability of the heart declines. Interestingly, studies have indicated that this type of cardiomyopathy can be potentially reversible. In instances where there are no other identifiable causes of heart dysfunction (like ischemia or valve disease), the heart may respond favorably to treatments like CRT. Reverse Remodeling: One of the most significant benefits of CRT is the phenomenon known as reverse remodeling, where the heart muscle regains its structural integrity and function after initiating CRT. Patients undergoing CRT often show improvements in heart chamber size—typically a reduction in the left ventricle’s diameter—along with enhanced pumping efficiency. As a result, not only can symptoms improve, but the overall prognosis for patients may also significantly enhance. Conduction System Pacing: A Specialized Approach Overview of Conduction System Pacing Conduction system pacing is an innovative technique in the field of cardiac pacing that aims to optimize the electrical activation of the heart. Unlike traditional pacing strategies that primarily stimulate heart chambers without addressing underlying conduction abnormalities, conduction system pacing focuses on restoring the natural conduction pathways. This method has shown particular promise in patients with left bundle branch block (LBBB)-related cardiomyopathy. The Mechanics of LBBP What is Left Bundle Branch Pacing (LBBP)?Left Bundle Branch Pacing (LBBP) is a specialized form of conduction system pacing where pacing leads are strategically positioned within the left bundle branch of the heart’s electrical system. This technique allows for direct stimulation of the left bundle branch to restore normal conduction patterns across the left ventricle. How Does LBBP Work? During normal heart function, electrical signals travel through the heart’s conduction system, ensuring that both ventricles contract in a synchronized manner. In LBBB, this pathway is disrupted, leading to asynchronous contractions and reduced cardiac efficiency. By placing a pacing lead in the left bundle branch, LBBP bypasses the damaged conduction pathway, promoting coordinated ventricular contraction that more closely resembles the heart’s natural rhythm. https://fuelforlife365.com/ Benefits of LBBP for Patients Improved Cardiac Function Clinical studies have shown that patients with LBBB undergoing LBBP frequently experience significant improvements in cardiac function. Enhanced synchronization of ventricular contractions leads to better overall heart performance, which can be measured through metrics such as increased ejection fraction and improved left ventricular volumes. Quality of Life Enhancements Alongside measurable improvements in heart function, patients often report a marked enhancement in their quality of life following LBBP. Symptoms such as fatigue, dyspnea (shortness of breath), and exercise intolerance may diminish significantly, allowing individuals to engage more fully in daily activities. Potential for Reverse Remodeling As mentioned earlier, one of the most promising aspects of CRT and LBBP is the potential for reverse remodeling. With effective pacing that restores normal electrical activity, the heart may regain its natural shape and improve function over time. This could alleviate the structural changes that typically accompany LBBB-related cardiomyopathy, further enhancing patient outcomes. … Read more